34 YRS OLD MALE WITH SOB, COUGH AND EXPECTORATION
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Hari Priya
Dr Govardini
Dr Sneha
- This is an online E-log to discuss our patient’s de-identified health data shared after taking his/her/guardian’s informed consent.
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
- I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
- The patient and the attenders have been adequately informed about the documentation and privacy of the patient. No identifiers shall be revealed throughout this presentation.
Patient came with chief complaints of B/L chest pain more on the left than on the right, associated with cough with expectoration and Shortness of breath since 3 months along with weight loss since 3 months, and decreased appetite since 2 years.
HISTORY OF PRESENTING ILLNESS :
- Patient was apparently asymptomatic 3 months back when he developed slight chest pain bilaterally which was 1- insidious in onset,
2- gradually progressing and
3- intermittent in nature
4- Aggravated on lifting heavy objects and weights
5- Relieved on resting.
6- pricking type pain, non radiating
7- no h/o palpitations, radiation of pain to right shoulder or shooting pains over left arm.
- Then he developed cough since 3 months that was sudden in onset, intermittent in nature associated with expectoration, usually of less quantity, light colored (mucus), No blood present in expectorant.
- Patient started to develop Shortness of Breath of grade II of MMRC since 3 months that was
1- insidious in onset,
2- gradual in progression
3- Aggravated on walking fast
4- Relieved on taking rest.
-All these symptoms were also accompanied by his sudden weight loss since 3 months, lost 15 kgs. His weight during April- May 2023 was 55kgs but has come down to 40kg at present.
- C/O low grade fever at night and partially early in the morning since 2-3 months, sudden in onset, occurring almost everyday, relieved on taking medication (typically T.DOLO 650mg)
-photo showing how loose his clothes are on him at present.
- This sudden h/o weight loss was also accompanied by a decrease in appetite, but that was present from 2 yrs, ever since he started consuming alcohol.
DAILY ROUTINE :
- He lives with his wife and has two adolescent kids who are at a hostel
- Patient is a farmer by occupation since 1.5 yrs. Before that he had a partnership with his friends 2 yrs ago over a wine shop with 25 % ownership over the same. However due to financial issues, he was unable to continue investing and was eventually dropped out from the business deal.
- Since he was in joint ownership with his friends he had access to unlimited alcohol hence started drinking about 1.5-2L of Whiskey namely on a daily basis. He used to have a good appetite before starting his consumption of alcohol but ever since starting 2 yrs ago, his appetite has decreased, but hasn’t experience any sort of weight loss unlike the past 3 months where he lost 15 kgs.
Prior to 2 yrs:-
- He usually starts off his day at 7am, usually having a cup of tea after brushing, followed by breakfast which includes a good portion of rice with vegetable curries.
- He is said to have consumed almost 5-6 meals prior to 2 yrs, stated he relatively had a better appetite then.
Since 2 yrs:-
- He usually starts around the same time as before, between 7-7:30 am he wakes up, brushes his teeth, takes his cup of tea and usually skips on breakfast and occasionally consumes alcohol during the mornings. He started drinking during morning time because of stress and fights he used to have with his wife at home. However despite that he still is able to work without any issue.
- He has been working as a farmer since 1.5 yrs. Usually ploughing paddy fields, spraying pesticides and works upto lunch. Usually has lunch at around 2pm, usually consuming a good portion of rice with vegetable curry. Occasionally indulges in non vegetarian items such as chicken, eggs and mutton twice to thrice a week, but doesn’t have much of a preference for fish.
- Usually comes home and consumes more alcohol either with his friends or alone. Doesn’t usually have dinner. Only occasionally has it. But has a preference for certain snacks such as rusk, biscuit etc.
- He complains of stress at home along with frequent arguments with his wife regarding his drinking which furthers leads to him drinking even more. Along with that has a bit of a financial issue at home as well.
PAST HISTORY :
- No similar complaints of cough, chest pain and SOB in the past
- Decreased appetite since 2 yrs (ever since he started consuming alcohol)
- No h/o HTN, DM II, TB, Bronchial Asthma, Epilepsy, CAD, CVA
ALLERGIC HISTORY:
-No h/o allergies or seasonal variation of symptoms
GENERAL PHYSICAL EXAMINATION:
- Patient is conscious, coherent and co-operative
- Pallor present
- No s/o icterus, cyanosis, clubbing, lymphadenopathy, edema
- Vitals at time of presentation-
BP: 120/80 mmHg
PR: 82 bpm
RR: 16 cpm
Temp: 98.2 F
SYSTEMIC EXAMINATION :
RESPIRATORY EXAMINATION-
I- Inspection-
- Chest is bilaterally symmetrical
- Trachea- midline position
- Chest normally moves with respiration
- No scars, sinuses or engorged veins
II- Palpation-
- No local rise of temperature
- Inspectory findings are confirmed
- Trachea- midline position
- Chest is moving equally on respiration on both sides
- Tactile Vocal Fremitus- equal on all areas.
III- Percussion-
Mammary- Resonant on both sides
Infra mammary- Resonant on both sides
Infra axillary- Resonant on both sides
Suprascapular- Resonant on both sides
Inter scapular- Resonant on both sides
Infra scapular- Resonant on both sides
IV- Auscultation-
- Bronchial breath sounds are heard
- No adventitious sounds heard.
CARDIOVASCULAR SYSTEM- S1S2 heard, no added murmurs
CENTRAL NERVOUS SYSTEM
- Conscious, coherent and co-operative
- Normal speech
- Reflexes- normal
- NAD
PER ABDOMEN :
- soft
- non tender
- no organomegaly.
DIAGNOSIS :
B/L ?Community Acquired Pneumonia
? Military Tuberculosis with Thrombocytopenia.
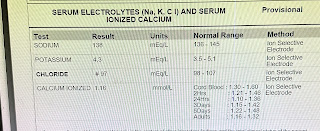
INVESTIGATIONS :
08/08/2023-
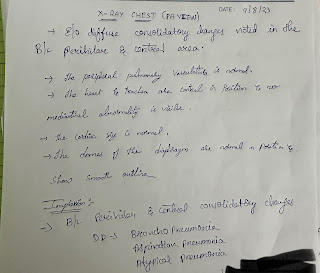
CHEST X-RAY PA VIEW
HAEMOGRAM-
RFT-
LFT-
RBS-
SEROLOGY- Negative
FEVER CHART-
09/08/2023
ESR
CHEST X-RAY PA VIEW REPORTING
10/08/2023
HAEMOGRAM
FEVER CHART
11/08/2023
FEVER CHART
TREATMENT :
08/08/2023
1. Inj AMOXYCLAV 1.2 gm IV/BD (8am—x—8pm)
2. IV fluids NS @75 ml/hr
3. Tan AZITHROMYCIN 500mg PO/OD (8am—x—x)
4. Inj PAN 40 mg IV/OD
09/08/2023
1. Inj AMOXYCLAV 1.2 gm IV/BD (8am—x—8pm)
2. Tan AZITHROMYCIN 500mg PO/OD (8am—x—x)
3. Inj PAN 40 mg IV/OD