45 YEAR OLD FEMALE WITH VIRAL PNEUMONIA SECONDARY TO COVID INFECTION
SNEHA CHAUHAN
ROLL NO 126
MBBS 8th SEMESTER
- This is an online E-log to discuss our patient’s de-identified health data shared after taking hi/her/guardian’s informed consent
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
Following is the view of my case-
CASE:
A 45 year old female came to the OPD with chief complaints of
- FEVER- since 1 week
- DRY COUGH- since 1 week
- LOSS OF APPETITE- since 1 week
- CHEST PAIN DURING DRY COUGH- since 2 days.
Past History :
Not a known case of Hypertension, DM, Epilepsy and CKD.
Drug History :
No significant drug history.
Personal History :
Diet: Mixed
Appetite: Decreased
Sleep: Adequate
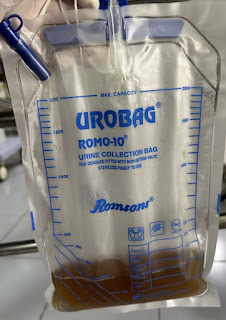
Bowel and Bladder movements: Regular
Addictions: None
Family History :
- No history of similar complaints in the family,
- No history of Diabetes, Hypertension, Heart disease, Cancers, Tuberculosis, Asthma, or any hereditary disease in the family.
General Examination :
- The patient is examined in a well lit room, with informed consent.
- The patient is conscious, coherent and cooperative at the time of examination.
Systemic Examination :
- Cardiovascular system- S1 and S2 heart sounds heard, no added murmurs or thrills.
- Respiratory system- Normal vesicular breath sounds heard
- Per Abdomen- soft, non tender, no organomegaly. Normal bowel sounds heard.
- Central Nervous System- Intact
Vitals :
Day1 - 11/05/2021 Day of admission
- Patient was conscious and coherent
- Pulse Rate (PR)- 88 beats/min
- Blood Pressure (BP)- 100/70 mm of Hg
- Respiratory Rate (RR)- 24 cycles/min
- Temperature- 98.6 ° F
- SPO2- 98% with 15 L of O2
Day 2- 12/05/2021
- Patient is conscious and coherent
- PR- 88 beats/min
- BP- 110/70 mm of Hg
- SP02- 99% with 10L of O2
- Temperature- 97°F
Day 3- 13/05/2021
- PR- 84 beats/min
- BP- 106/70 mm of Hg
- SPO2- 96% with 10L of O2
Day 4- 14/05/2021
- Patient is conscious and coherent
- PR- 90 beats/min
- Temperature- 98.4°F
- SPO2- 90-98% with 10L of O2
- Complains of- Dry mouth and Breathlessness
Day 5- 15/05/2021
- PR- 86 beats/min
- BP- 110/70 mm of Hg
- Temperature- Afebrile
- SPO2- 99% with 15 L of O2
Day 6- 16/05/2021
- Patient is conscious, coherent and cooperative
- PR- 97 beats/min
- BP- 120/80 mm of Hg
- SPO2- 98%
- RR- 22 cycles/min
- GRBS- 205 mg/dl
Day 7- 17/05/2021
- Patient is conscious, coherent and cooperative
- PR- 89 beats/min
- BP- 110/60 mm of Hg
- Temperature- Afebrile
- SPO2- 96% on 10L of O2
Day 8- 18/05/2021- Day of discharge
- Patient is conscious, coherent and cooperative
- PR- 86 beats/min
- BP- 110/70 mm of Hg
- SPO2- 95% on 2L of O2
- Temperature- Afebrile
Investigations :
- CBP
- Haemoglobin- 12.9 g% (normal range- 13-17 g%)
- Total Leukocyte count- 4000 cells/cumm
- Differential Leukocyte count-
- Neutrophils : 67 % ( normal- 40-80)
- Lymphocytes : 28% (normal- 20-40)
- Eosinophils : 2% (normal- 1-6)
- Monocytes : 3% (normal- 2-10)
- Platelet count- 1.51 lakh/cumm (normal range— 1.5-4.1)
- Haemoglobin- 12.3 g%
- Total Leukocyte count- 10,500
- Differential Leukocyte count-
- Neutrophils : 63%
- Lymphocytes : 11%
- Eosinophils: 3%
- CRP- On 11/05/2021– Positive 0.6 mg/dl
- D-Dimer- On 11/05/2021- 1150 ng/ml (normal range < 200 ng/ml)
- LFT-
- ALP (Alkaline Phosphate) : 106 IU/L (normal range- 53- 128)
- SGOT (AST) : 41 IU/L (normal range- 0-35)
- SGPT (ALT) : 40 IU/L (normal range- 0-45)
- Total Proteins : 6.2 g/dl (normal range- 6.4-8.3)
- RFT- Normal
- Serum LDH- 518 IU/L ( normal range- 140-280)
- X ray Chest
- On 11/05/2021 at 6:45pm
- On 17/05/2021 at 9:45 pm
- ECG-
Provisional Diagnosis :
Viral Pneumonia secondary to COVID-19 infection.
HRCT- CORADS 5
CT score- 6/25
Treatment Regimen : (11/05/2021- 18/05/2021)
- IVF—75ml/hr Inj. OPTINEURON
- O2 supplementation to maintain SPO2 > 90%
- Nebuliser- Duolin, Budefort, every 6th hourly
- Inj. PANTOP 40mg IV/OD
- Tab MVT OD
- Tab LIMCEE OD
- Tab DOLO 650mg
- Syp GRILLINCTUS 2tsp 1-1-1
- Inj. DEXAMETHASONE 8mg/IV/OD
- Inj. CLEXANE 40 mg SC/BD
- Pulse rate, Blood pressure, and SPO2 monitoring hourly
- Temperature charting every 4th hourly
Additional medication-
11/05-2021
- GRBS monitoring every 6th hourly
12/05-2021
- Inj. CLEXANE 40mg/SC/BD started
13/05-2021
- Inj. HAI 4U-4U-4U started
15/05-2021
- GRBS monitoring every 2nd hourly
16/05-2021
- Inj. HAI increased to 8U-8U-8U
- Tab SPOROLAC TID
- ORS
18/05-2021
- Tab SPOROLAC stopped
- ORS stopped
- Syrup CREMAFFIN given
Patient was discharged on 18th May 2021, at 5pm.
Duration of stay- 8 days.
Questions-
Q1. Is there a relation between Covid-19 infection and serum LDH levels?
Q2. Despite being not a known case of Diabetes, what is the reason for her GRBS being high?
Under the guidance of Dr. Sai Charan Sir.