36 YEAR OLD MALE WITH ANGIOEDEMA
SNEHA CHAUHAN
ROLL NO- 126
2017 BATCH
9th SEMESTER
PREFINALS PRACTICAL CASE BLOG
- This is an online E-log to discuss our patient’s de-identified health data shared after taking his/her/guardian’s informed consent.
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
- I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
- The patient and the attenders have been adequately informed about the documentation and privacy of the patient. No identifiers shall be revealed throughout this presentation.
A 36 year old male who is a, watchman by occupation, was brought to the AMC at 4am by his brother on Wednesday 12th January 2022, with chief complaints of
Chief complaints
- Discomfort of the throat followed by
- Swelling and pain of the throat since 3 hours from onset of symptom
History of Presenting Illness-
- The patient experienced discomfort in the throat at around 1am, during the morning of 12/01/22, whilst working. He went to check himself in the mirror in order to examine what was wrong and noticed his throat starting to swell up.
- The patient noticed the swelling starting at the base of the tongue and around the uvula, which eventually progressed down.
- He felt as if the whole of his throat was swelling up.
The swelling was-
- Sudden in onset
- Rapid in progression in a matter of a few hours,
- Associated with
Pain-
- Was sudden in onset
- Rapidly progressing to the point where he was unable to even turn his neck side to side.
- Not much associated with difficulty in breathing at that time of swelling.
Past history-
- The patient has had similar complaints in the past.
- He was apparently asymptomatic 15 years back (before 2007), when he first developed similar complaints of swelling of the throat associated with pain and difficulty in breathing because of said swelling for which he went to the local hospital and was referred to our hospital and a tracheostomy was done to relieve that.
- Along with the throat swelling, patient also experienced multiple episodes of generalised swelling across the body which often appeared first in a specific site, and would rapidly progress throughout the body.
- Not associated with any itching, redness, bleeding.
- The generalised swelling often persisted for 3 days, and when taking medication (hydrocortisone), it would reduce faster, approximately within 5-10 hours.
- The frequency of how often the generalised swelling used to occur would be intermittent and random, about 2 episodes at most per month.
- The generalised swelling usually occurred on the face, upper and lower limbs, and the trunk. Commonly, the face and the extremities.
- In 2016, he had a second episode of the similar complaint of swelling of the base of tongue and uvula (throat region), for which a tracheostomy was done once again.
- Onset of these symptoms made it difficult for him to go to work consistently, hence the need for medications to relieve some of the symptoms.
- Patient does not have diabetes, hypertension, asthma, tuberculosis, epilepsy.
Allergic history-
- Patient is said to be allergic to Food items such as fish, mutton, brinjal
- And is sensitive to smell and scents such as sanitizer, garbage,
- Pollutants, smoke and dust.
Family history
No history of similar complaints in the family.
Treatment history-
Takes Avil and Hydrocortisone injection from time to time, whenever an attack of swelling occurs
Surgical history-
Tracheostomy done twice till date.
Personal history-
- Mixed diet (excluding the foods he is allergic to)
- Normal appetite
- Inadequate sleep due to his field of work
- Regular bowel and bladder movement
- No such habits of alcohol consumption or smoking alike.
General physical examination-
Patient is conscious, coherent and cooperative.
VITALS-
- Heart rate- 120 beats per minute
- Respiratory rate- 16 cycles per minute
- Temperature- Afebrile
- Blood pressure- 120/91 mmHg
No signs of pallor, icterus, clubbing, lymphadenopathy, cyanosis,
Edema of extremities are absent
Edema of uvula and tongue are seen.
ENT and Respiratory examination-
- Examination of nose and oral cavity-
- No trismus
- Examination of oral cavity- lips, teeth, gums, buccal mucosa, Gingivobuccal sulcus (upper and lower), gingivolingual sulcus (upper and lower), Retromolar trigone, Anterior 2/3rd of tongue, hard palate and floor of mouth all appear normal.
- Examination of oropharynx- oedema and congestion of anterior pillar, uvula and soft palate, posterior pharyngeal wall appears congested.
- Examination of nose- turbinates and mucosa appear normal.
- Examination of neck shows Tracheostomy scar, and normal neck movements.
2. Inspection of chest-
- Shape of chest- Bilaterally symmetrical
- Expansion of chest- appears equal on both sides
- No crowding of ribs
- No visible pulsations or engorgement
- No kyphoscoliosis
- No visible scars or sinuses.
3. Palpation of chest-
- No tenderness
- No local rise of temperature
- Expansion of chest equal on both sides
- Apex beat- medial to mid clavicular line in 5th intercostal space
4. Percussion- resonant on all areas of percussion
5. Auscultation- bilateral air entry present, normal vesicular breath sounds
Abdominal examination-
- Inspection- shape of abdomen is scaphoid, no visible peristalsis
- Palpation- soft, non tender and no organomegaly
- Percussion- no free fluid
- Auscultation- bowel sounds heard.
Cardiovascular system examination-
- Inspection- no visible pulsation
- Palpation- apex beat felt
- Percussion- heart borders are normal
- Auscultation- S1S2 heard, no added murmurs
Central nervous system examination-
- Conscious
- Normal speech
- Cranial nerves intact
- Sensory and motor system- normal
- Neck stiffness- absent
- Reflexes- normal
Investigations-
- Haemoglobin- 13g/dl
- Total Leukocyte count- 13,200 cells/cumm
- Platelet count- 4.6 lakhs/cumm
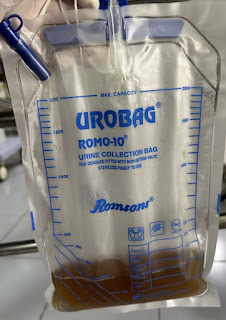
- Complete Urine examination- no sugars, no albumin present.
- Blood grouping- A positive
- Random Blood Sugar- 115mg/dl
- RFTs-
- Urea- 19
- Creatinine- 1
- Sodium- 140 mEq/L
- Potassium- 4.1 mEq/L
- Chloride- 94 mEq/L
8. Liver Function Tests-
- Total bilirubin- 1.19 mg/dl
- Direct bilirubin- 0.3mg/dl
- AST(SGOT) - 25 IU/L (N 5-40)
- ALP(SGPT) - 145 IU/L (N 44-147)
- ALT- 21 IU/L (N 7-55)
9. C4 complement serum
11. ECG