50 YEAR OLD MALE CAME WITH ABDOMINAL DISTENSION AND SOB
Unit posting (Intern 2017)
Medical Ward
GM II
Dr Nikitha
Dr Pavan
Dr Lohith
Dr Sneha
- This is an online E-log to discuss our patient’s de-identified health data shared after taking his/her/guardian’s informed consent.
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
- I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
- The patient and the attenders have been adequately informed about the documentation and privacy of the patient. No identifiers shall be revealed throughout this presentation.
PREVIOUS ADMISSION CASE
A 50 year old Male came with chief complaints of abdominal distension since 4 days associated with shortness of breath.
TIMELINE OF EVENTS & DAILY ROUTINE-
- Around February 2023, an ASHA worker had visited the patient in his area for a routine check up and had noticed and mentioned to the patient about the yellowish discolouration of his eyes
- for which he got it checked at a local nearby hospital and was given conservative management for the same for which the symptoms were relieved
- Sometime in April 2023, patient then developed distension of abdomen that was insidious in onset, gradually progressing associated with shortness of breath (grade 2 of MMRC) [ not associated with chest pain, palpitations, vomiting, loose stools, orthopnea, fever, cough, cold, burning micturition, PND],
-for which he was admitted into our hospital where he got treated conservatively along with a therapeutic ascitic tap that was done.
- Ever since then, he has stopped consuming alcohol and moved to a more vegetarian diet.
HISTORY OF PRESENTING ILLNESS-
Presently, patient is a case of chronic liver disease who is on regular medication who came with
- abdominal distension- insidious in onset, gradually progressive associated with Shortness of breath- of grade II type ie walks slower than usual and usually stops to catch his breath (MMRC).
- no h/o fever, cold, cough, chest pain, orthopnoea, PND, vomiting
PAST HISTORY-
-No history of Hypertension, Diabetes Mellitus, CVA, Tuberculosis, Asthma.
- no past surgical history.
- no h/o allergies.
- During us admission 3 months back, an endoscopy was done i/v/o Oesophageal varices
PERSONAL HISTORY-
DIET- Presently a more vegetarian based diet
APPETITE- Normal
BOWEL AND BLADDER MOVEMENT- regular
SLEEP- adequate
HABITS- Stopped alcohol consumption 4 months ago. Otherwise was a chronic alcoholic for 20 years, namely consuming Sara, a country alcohol having about 25 to 45 % alcohol content
FAMILY HISTORY- Insignificant
GENERAL PHYSICAL EXAMINATION-
- Well built and moderately nourished
- Weight : 60kgs
- Height : 164 cm
- Pallor present
- Icterus present
- No s/o edema, lyphmoedema, cyanosis, clubbing.
VITALS-
- Pulse Rate : 82 bpm
- Respiratory Rate : 16 cpm
- Blood Pressure : 110/60 mmHg
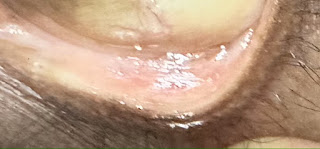
Dupuytren’s contracture seen on left hand of patient-
SYSTEMIC EXAMINATION -
1. ABDOMINAL EXAMINATION :
Inspection :
- Shape of abdomen - Distended
- umbilicus - Central and inverted
- no visible peristalsis
- no scars or sinuses seen.
Palpation :
- non tender
- Spleen - palpable
- Abdominal girth- 88cm
Percussion :
- Shifting dullness - present
- Fluid thrill - absent
Auscultation :
- no bowel sounds heard.
Cardiovascular system examination-
- Inspection- no visible pulsation
- Palpation- apex beat felt
- Percussion- heart borders are normal
- Auscultation- S1S2 heard, no added murmurs
Central nervous system examination-
- Conscious
- Normal speech
- Cranial nerves intact
- Sensory and motor system- normal
- Neck stiffness- absent
- Reflexes- normal
Respiratory examination-
- examination of nose and oral cavity- appear normal
- Inspection-
- Shape of chest- bilaterally symmetrical
- Expansion of chest- appears equal on both sides
- No crowding of ribs
- No visible pulsation or engorgement
- No visible scars or sinuses
- Palpation of chest-
- No tenderness
- No local rise of temperature
- Expansion of chest equal on both sides
- Apex beat- medial to mid clavicular line in the 5th intercostal space.
- Percussion-resonant on all areas
- Auscultation- Bilateral air entry, normal vesicular breath sounds.
DIAGNOSIS : Chronic Liver Disease
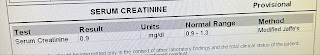
INVESTIGATIONS DONE :
On 13/06/2023-
- Irregular and coarse echo texture of Liver
- Mild splenomegaly
- Gross Ascites (s/o chronic liver disease)
14/06/2023
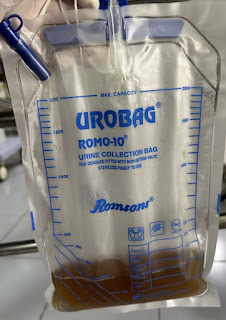
Diagnostic Ascitic tap done of around 1000ml -
15/06/2023-
16/06/23-
Ascitic tap was done of around 500ml
17/6/23-
- Therapeutic Ascitic tap of 1L was done
TREATMENT GIVEN-
1. Water restriction less than 1.5 L/ day
2. Salt restriction less than 2g/day
3. Tab ALDACTONE 50 mg PO OD
4. Tab PAN 40 mg PO/OD BBF
5. Syp LACTULOSE 30 ml before bed
6. Syp POTKLOR 15 ml in 1 glass of water PO/BD
7. Consume 2 egg whites/ day
8. Monitor vitals
Patient was discharged after 5 days of admission. Advised the same treatment given during the duration of stay at hospital as well as the need for a liver transplant.
THEORY : (images taken from Cancer Research UK)