Unit posting (Intern 2017)
AMC Bed no-2
GM II
Dr Nikitha
Dr Pavan
Dr Lohith
Dr Sneha
- This is an online E-log to discuss our patient’s de-identified health data shared after taking his/her/guardian’s informed consent.
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
- I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
- The patient and the attenders have been adequately informed about the documentation and privacy of the patient. No identifiers shall be revealed throughout this presentation.
Patient complaints of fever since 3 days, SOB since 2 days and loose stools today.
HISTORY OF PRESENTING ILLNESS-
Patient was apparently asymptomatic 3-4 days ago, then she developed low grade fever, intermittent nature, relieved on iv medication, associated with generalized weakness associated with SOB since 2 days (Grade 4 of MMRC at time of presentation)
- No h/o palpitations, chest pain, cold, cough, burning micturition, and rashes.
- Has h/o abdominal bloating and discomfort and c/o loose stools of low volume, not associated with pain abdomen.
- loose watery stools 3-4 episodes today.
HER DAILY ROUTINE-
- She’s a coolie by occupation, works 8-5 daily, consumes rice in all three meals and often complained of body pains due to her field of work so used to consume non- prescribed pain medications (unknown).
- She had complained of fever 3 days prior to her visit to our hospital, for which she had gone to a RMP doctor who prescribed her medication for her fever along with IV fluids. Her symptoms were relieved then.
- a day before her visit to our hospital she had complained of abdominal pain for which she visited a local hospital who referred her to us.
PAST HISTORY-
- no h/o similar complaints in the past
- no h/o DM, HTN, Asthma, Epilepsy, Tuberculosis, CVA, CAD
GENERAL PHYSICAL EXAMINATION-
- well built and nourished
- No signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy and edema
- Vitals
Pulse rate- 120 beats per minute
Respiratory rate- 36 cycles per minute
Temperature- Afebrile
Blood pressure- 90/60mmHg
GRBS- 96mg/dl
SYSTEMIC EXAMINATION-
Abdominal examination-
- Soft, non tender,
- no organomegaly
- Bowel sounds present
Cardiovascular system examination
•S1 and S2 heard , no added thrills and murmurs heard.
Respiratory system examination
- BLAE present
- NVBS
- On Auscultation- crepitations heard on B/L infra axillary region, and Infra scapular region, Right more than left side.
Central nervous system examination-
- Conscious
- Normal speech
- Cranial nerves intact
- Sensory and motor system- normal
- Neck stiffness- absent
- Reflexes- normal
DIAGNOSIS-
- Septic Shock with Community Acquired Pneumonia with Acute Kidney Injury
INVESTIGATIONS-
14/06/2023
ABG at 9:30 am
ABG at 8:30 pm
USG FINDINGS (IMPRESSION) -Minimal Ascites noted.
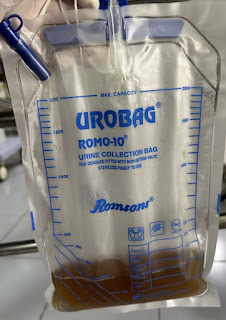
Urine culture and sensitivity- no significant growth.
Blood culture- Gram Negative organism isolated
15/06/2023
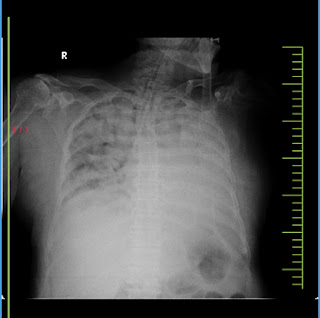
Bedside chest X-ray
- E/O radio-opacities notes in B/L lung fields, predominantly noted in the lower lobes
- Right hilar enlargement noted
- heart and trachea are central
- the diaphragm show smooth outline
Impression- Consolidatory changes noted in B/L lung fields.
Haemogram-
Serum Electrolytes-
ABG at 8am-
pH- 7.385
pCO2- 21.6 mmHg
pO2- 53.5 mmHg
cHCO3- 15.9 mmol/L
Sr creatinine-
Sr Urea-
16/06/2023-
ABG done at 4am-
pH- 7.340
pCO2- 21.7 mmHg
pO2- 63.3 mmHg
cHCO3- 13.5 mmol/L
Hemogram-
Serum electrolytes with urea and creatinine-
Blood lactate-
Blood culture- E.Coli isolated (sensitive to Cotrimoxazole, Piperacillin/Tazobactam, Meropenam.)
2D ECHO-
- mild to moderate MR, moderate AR, mild TR
- no RWMA, No AS/MS, sclerotic AV
- Good LV systolic function
- diastolic dysfunction, no PE
17/6/23-
- Serum Electrolytes with urea and creatinine
- chest X-ray sitting position
Intubation done on 17/6/23 at 3:30pm due to oxygen desaturation.
Post intubation ABG-
pH- 7.210
pCO2- 30.9 mmHg
pO2- 42.1 mmHg
HCO3- 12.9 mmol/L
Post intubation chest X-ray
Fever chart-
TREATMENT-
1. IV Fluids NS @ 100ml/hr
2. Inj MONOCEF 1gm IV BD
3. Inj PAN 40mg IV OD
4. Inj 25 D if GRBS- 60mg/do
5. Temperature charting every 4th hourly
6. Monitor vitals
7. Inj.Piptaz 1gm IV BD / day 3
On 17/6/23-
1. IV FLUIDS - NS, RL @100ML/HR
2. (DAY 4) INJ PIPTAZ 2.25GM IV TID
3. (DAY 3) TAB AZITHROMYCIN 500MG PO OD
4. INJ PANTOP 40MG IV OD
5. INJ 25D IV STAT IF GRBS <60MG/DL
6.BP,PR, SPO2, RR CHARTING HOURLY
7. TEMP MONITORING 4TH HOURLY
8.STRICT I/O CHARTING
9. ORS SATCHET IN 1LITRE WATER AFTER EVERY LOOSE STOOL EPISODE
Patient expired on 17/06/2023 at 6:21 pm-
Due to sudden bradycardia with no central and peripheral pulses, CPR was initiated according to ACLS guidelines and was continued for 30 minutes despite which patient could not be resuscitated and was declared dead at 6:21pm on 17/6/23 with ECG showing no electrical activity.
Immediate cause of death- Type 1 respiratory failure with refractory metabolic acidosis
Antecedent cause of death- Acute Respiratory Distress Syndrome with Septic Shock with MODS with ?DIC