65 YEARS OLD MALE CAME WITH PEDAL EDEMA, FACIAL PUFFINESS, SOB AND HOARSENESS OF VOICE
2017 batch
ICU bed 4 & DIALYSIS UNIT
DR.PAVAN
DR. NAVYA
DR.SNEHA
DR. NAVYA
DR.SNEHA
- This is an online E-log to discuss our patient’s de-identified health data shared after taking his/her/guardian’s informed consent.
- Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
- This E-log also reflects my patient centered online learning portfolio and your valuable inputs on comment box are welcome.
- I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis” to develop my competence in reading and comprehending clinical data including history, clinical findings and come up with diagnosis and treatment plan.
- The patient and the attenders have been adequately informed about the documentation and privacy of the patient. No identifiers shall be revealed throughout this presentation.
Patient came with chief complaints of pedal edema since 2 days, associated with facial puffiness since 2 days, shortness of breath (Grade II of MMRC) since 2 days and hoarseness of voice since 2 days.
TIMELINE OF EVENTS & DAILY ROUTINE-
- Patient’s usual daily routine is that he typically wakes up at around 6-7AM, gets ready for the day and usually just goes to the milk shop to collect milk, comes home, eats breakfast and works occasionally as a farmer in paddy fields.
- Patient works occasionally on and off to keep his mind occupied, usually has lunch at around 1-2 pm, takes a small nap and then starts his social activities with neighbors and family members.
- Usually has dinner on time with his family and goes to bed by 10.
- Patient was fine, living his normal routine life up until 2017 where he was diagnosed to have hypertension and was given medication for the same during a routine general check up.
- Patient noticed both his ankles and feet swelling associated with SOB of grade II of MMRC back in 2018, was diagnosed with Chronic Renal Failure and as per the advice of his physician at the time, he was asked to stop anti-hypertensive drugs altogether, and given conservative treatment for the CKD (which was Prolomet XL along with an antacid and vitamin supplements)
HISTORY OF PRESENT ILLNESS-
- Patient was apparently asymptomatic until 2 days ago where he developed Pedal edema which was sudden in onset, gradually progressing, since 2 days of pitting type below the knees
- Associated with facial puffiness, which was insidious in onset, gradually progressing, no aggravating of relieving factors.
- and Shortness of breath (grade II of MMRC) along with hoarseness of voice, that was insidious in onset, gradual in progression, no aggravating or relieving factors.
- not associated with cough, cold, fever, chills, palpitations, sweating, decreased urine output, blood in urine.
PAST HISTORY-
- H/O HTN since 2017, was on regular medication till 2018 then stopped as per the advice of his physician but has been prescribed Prolomet XL (metoprolol combination drug)
- No H/O DM, Thyroid disorders, Asthma, Epilepsy, TB, CVA, CAD
PERSONAL HISTORY-
DIET- Currently consuming more of a non vegetarian diet
APPETITE- Normal
BOWEL AND BLADDER MOVEMENT- regular
SLEEP- adequate
HABITS- only used to consume half to one litre of toddy occasionally during functions 20 years back. No present day addictions as such.
FAMILY HISTORY- insignificant
GENERAL PHYSICAL EXAMINATION:
- Patient is conscious, coherent and cooperative.
- Well built and moderately nourished
- height- 178cm
- weight- 78kgs
- pallor- present
- no signs of icterus, clubbing, lymphadenopathy
- at time of doing this blog, patient has received treatment and dialysis for which most of his symptoms including pedal edema have subsided to a major extent so no signs of edema presently.
PR- 82bpm
BP- 130/70 mmHg
RR- 22cpm
SpO2- 98% on RA
Temp- 98.4 F
SYSTEMIC EXAMINATION-
Cardiovascular examination :
- inspection- No previous surgical scars, sinuses, no apical
Impulse seen
- palpation- Apex beat is medial to mid clavicular line between 4-5th intercostal space.
- auscultation- S1S2 heard, no murmurs present.
Respiratory examination-
- inspection- no previous scars, sinuses or engorged veins; expansion of chest appears equal, no appearance of broken ribs, position of trachea appears central.
- palpation- expansions of chest equal on both sides, no rise in temperature, Inspectory findings confirmed
- percussion- Resonant on all areas
Anterior- Clavicular (direct); Mammary and infra mammary (indirect)
Lateral- mid axillary line (6th ICS)
Posterior- Supra and infra scapular; mid scapular (superior, middle and inferior)
Per Abdomen-
- at the time of presentation, it was distended on appearance but after treatment was given, it is scaphoid in shape,
- soft, non tender
- no organomegaly.
Central Nervous Examination- Higher motor functions intact. No abnormal findings
PROVISIONAL DIAGNOSIS- Chronic Renal Failure
INVESTIGATIONS-
28/06/2023-
29/06/2023-
USG ABDOMEN :
- Right Grade II RPD Changes
- left grade III RPD changes
- b/l renal cortical cysts
ECG :
30/06/2023-
2D- ECHO
- No RWMA
- no AS/MS
- sclerotic AV
- Good LV systolic function; diastolic dysfunction present
03/07/2023-
TREATMENT GIVEN -
1. Tab NODOSIS 500 mg PO/OD
2. Tab LASIX 40 mg PO/BD
3. Tab OROFEE XT PO/OD
4. Tab SHELCAL PO/OD
5. Cap BIO D3 PO once a week
6. INJ EPO 4000 IV/SC once a week
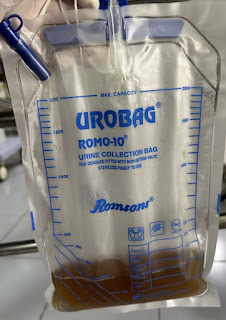
7. Dialysis done on 3/7/23
- Patient got discharged on 4/7/23.
Patient was readmitted for a dialysis to be done on 8/7/23
8/7/23
-During dialysis patient developed Shortness of Breath along with chills and fever.
- after his dialysis patient seemed alright and was shifted to ward and was stable for a while,
- after which he was unconscious with his BP coming to 60/40 mmHg for which he was shifted to ICU and 300 ml bolus was given.
09/07/2023
- Patient was shifted to the CKD ward
10/07/2023-
11/7/23-
13/7/23
1. Tab NODOSIS 500 mg PO/OD
2. Tab LASIX 40 mg PO/BD
3. Tab OROFEE XT PO/OD
4. Tab SHELCAL PO/OD
5. Cap BIO D3 PO once a week
6. INJ EPO 4000 IV/SC once a week
- Patient got discharged on 14/7/23.