Introduction:
This online E-log Entry Blog is an objectively structured clinical examination method to assess the clinical competence during the course of my General Medicine Internship rotation (June'2023-August'2023) by reviewing the case reports shared below and to discuss, understand and review the clinical scenarios and data analysis of patients so as to develop my clinical competency in comprehending clinical cases, and providing evidence-based inputs for questions surrounding the clinical vignettes borrowed from the E Log Book.
The cases have been shared after taking consent from the patient/guardian. All names and other identifiers have been removed to secure and respect the privacy of the patient and the family.
CASE REPORT 1:-
https://snehachauhan126.blogspot.com/2023/06/60-f-came-with-fever-and-loose-stools.html
Patient came with complaints of fever since 3 days along with SOB since 2 days and 3-4 episodes of loose stools on the day of admission.
GENERAL APPROACH TO PATIENT :
1- Timeline of events before and after admission and list all complaints with relevant clinical data pertaining to the case along with treatment plan for each that was done to aid in patient relief.
A- The general timeline of events before and after admission summary.
BEFORE ADMISSION-
- Patient is someone who regularly uses pain medications (unknown) according to her family members as she’s a coolie by occupation and often has generalized body pains due to her profession
- Had fever 3 days prior to admission and visited RMP and was given IV fluids and prescribed medication. Symptoms were briefly relieved then.
- A day prior to admission, patient complained of abdominal pain and was referred to our hospital.
AFTER ADMISSION-
- Patient was conscious, coherent and co-operative
- Low grade fever, intermittent in nature, relieved on iv medication (namely paracetamol IV along with IV fluids to help with her dehydration.)
- associated with Grade 4 of MMRC SOB (patient was started on oxygen mask which later progressed to CiPAP and later on to being intubated after 4 days from admission.)
- generalized weakness
- h/o abdominal discomfort with 3-4 episodes of loose stools of low volume, watery consistency.
- Respiratory examination- on auscultation B/L infra axillary region and infra scapular region, crepitations heard, Right >>left.
Serum Creatinine and Blood urea trend:
- Patient’s blood culture report shows Escherichia coli isolated (was started Inj PIPTAZ 1gm IV BD)
- Patient’s Urine culture was negative for any microbial growth.
- Patient was intubated due to oxygen de-saturation.
- Diagnosis: Septic Shock with Community Acquired Pneumonia with Acute kidney Injury.
- Plan for dialysis on day 4 of admission.
PATIENT SPECIFIC APPROACH:-
1- Pathophysiological progression of the patient with respect to the events that may have taken place owing to her condition.
- E.COLI could have been acquired from three ways.
1. From contaminated foods
2. ARDS as a result of disseminated bacteremia
3. And could progress to HUS (Hemolytic Uremic Syndrome).
- all of the above three possible scenarios lead to bacteremia ie bacteria entering the blood stream.
- which results into release of toxins leading to septic shock and AKI with Organ Dysfunction.
(With reference to image taken from Cleveland Clinic)
2- What other tests should have been ordered which could have aided in understanding the onset of the progression of the disease?
A- two additional tests could have been done ie-
1) Stool test- For understanding the strain of E.Coli
2) A peripheral blood smear- for checking if there’s any hemolysis.
3- Why is Hemolysis something to be checked by a peripheral smear and what’s its relevance?
A- Hemolysis is a feature of HUS ie Hemolytic Uremic Syndrome.
- it can be a provisional diagnosis as Hb decreases along with PCV decrease from the day of admission with reference to the Haemogram trend, however that can also be attributed to giving IV Fluids hence the need to rule out hemolysis through Peripheral smear.
- Apart from that, why HUS has come in the picture is because of the urea and creatinine trend, associated with the patient’s complaints and progression of disease.
- however it is the least likely provisional as
urine culture shows
no microbial growth.
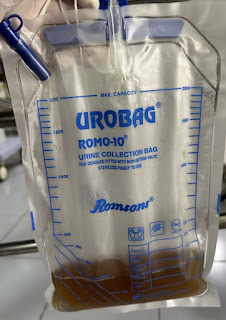
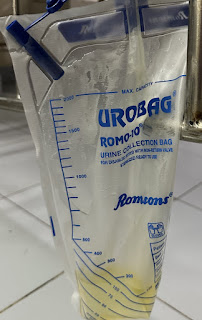
4- Any significance in the change of urine from day of admission to after admission? And what intervention may have changed it along with why is urine appearance important in this case?
A-
BEFORE ADMISSION :
- High colored urine usually as a result of dehydration.
AFTER ADMISSION :
Pale yellow color, as a result of IV fluids administration to help with her dehydration.
- The reason why urine is of importance is to further help rule out HUS. If hemolysis was present, hematuria may be a usual symptom. However at the day of admission, high colored urine may be confused for hematuria.
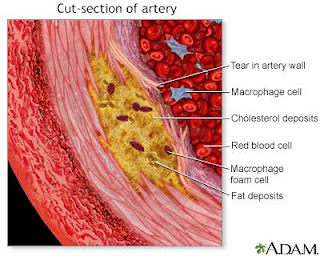
5- How does visceral fat contribute to organ damage at a molecular level?
A-
- Visceral fat generally has basic risks usually as a result of High cholesterol, Type II DM, Heart disease etc.
- basic risk of it is the deposition of cholesterol in the blood vessel lining, leading to its eventual block over time.
(Image taken from ADAM)
Complications include- Stroke, MI etc.
6- Progression of her SOB.
A-
CHEST X-RAY-
14/6/23
15/6/23
17/6/23
- before intubation
- after intubation
ABG TRENDS-